HIPAA Quizzes, Questions & Answers

HIPAA (The Health Insurance Portability and Accountability Act) Quizzes, Questions & Answers
Why don’t you start by checking your level of awareness through these HIPPA quiz answers? Are you familiar with the terminologies and rules involved? What are the possible violations that people are likely to encounter? How can one protect their company as well as provide what’s best for their customers? Do you think you’re up to the task? To compliance and beyond! There’s no turning back now! Start off with these HIPPA quiz questions and answers!
Trivia Questions On HIPAA, Privacy And Confidentiality! Quiz

Questions and Answers
-
1. Which of the following is NOT a best practice for privacy and security?
-
A. Keeping fax machines in areas that are not generally accessible
Correct Answer
C. Documents containing PHI do not need to be shreddedExplanation
It is not a best practice for privacy and security to not shred documents containing PHI (Protected Health Information). Shredding documents that contain sensitive information helps to prevent unauthorized access and protects individuals’ privacy. It ensures that the information cannot be easily reconstructed or used maliciously. Therefore, it is important to shred documents containing PHI to maintain privacy and security.2. You always abide by the HIPAA privacy rule.
Correct Answer
B. FalseExplanation
The statement “You always abide by the HIPAA privacy rule” is incorrect. It is not possible for someone to always abide by the HIPAA privacy rule as it requires continuous effort and adherence to the regulations set forth by HIPAA. Compliance with HIPAA is an ongoing process that involves regular training, updates, and implementation of privacy measures. Therefore, the correct answer is False.A. TrueB. False -
-
3. PHI stands for Private Health Information.Correct Answer
B. FalseExplanation
PHI stands for Protected Health Information, not Private Health Information. Protected Health Information refers to any information about a person’s health status, medical conditions, treatment, or payment for healthcare services that can be linked to an individual. It is important to protect PHI to ensure patient privacy and comply with HIPAA regulations. Therefore, the correct answer is False.A. TrueB. False -
4. Clients need to receive a copy of the Notice of Privacy Practices.
-
B.
False
Correct Answer
A. TrueExplanation
Clients need to receive a copy of the Notice of Privacy Practices because it is a legal requirement under the Health Insurance Portability and Accountability Act (HIPAA). The Notice of Privacy Practices outlines how an organization handles protected health information, including how it is used, disclosed, and protected. By providing clients with a copy of this notice, they are informed about their privacy rights and can make informed decisions about their healthcare.A. True
-
-
5. Confidentiality means that data is not to be made available to unauthorized persons.
-
B.
False
Correct Answer
A. TrueExplanation
Confidentiality refers to the practice of keeping sensitive information private and secure, ensuring that it is only accessible to authorized individuals. This principle ensures that data is not disclosed or shared with unauthorized persons, protecting it from potential misuse or unauthorized access. Therefore, the statement “Confidentiality means that data is not to be made available to unauthorized persons” is true as it accurately reflects the concept of confidentiality.A. True -
-
6. How many major concepts are associated with the privacy rule?
-
A. One
-
B. Two
-
C. Three
-
D. Four
Correct Answer
B. TwoExplanation
The correct answer is Two. The privacy rule is associated with two major concepts. These concepts include the use and disclosure of protected health information (PHI) and the individual’s rights regarding their PHI. The rule outlines how PHI can be used and disclosed by covered entities, as well as the rights of individuals to access, amend, and request restrictions on the use of their PHI. By understanding these two concepts, organizations can ensure compliance with the privacy rule and protect individuals’ privacy rights. -
-
7. Which of the following information is generally considered confidential?
-
A. Demographics
-
B. Diagnosis
-
C. Billing Information
-
D. Dates of Service
-
E. All of the Above
Correct Answer
E. All of the AboveExplanation
All of the information listed – demographics, diagnosis, billing information, and dates of service – is generally considered confidential. Demographics such as age, gender, and address can be used to identify individuals. Diagnosis and medical conditions are sensitive personal information that should be kept private. Billing information includes financial details that should be protected. Dates of service can reveal when and where a person received medical treatment, which is also considered confidential. Therefore, all of the above options are generally considered confidential information. -
-
8. A person’s phone number is not considered PHI because it can be located in an online or paper telephone directory.
-
A. True
-
B. False
Correct Answer
B. FalseExplanation
A person’s phone number is considered PHI (Protected Health Information) because it is a unique identifier that can be used to identify an individual’s health information. Even though phone numbers may be publicly available in telephone directories, when they are linked to an individual’s health information, they are protected under HIPAA regulations. Therefore, the statement that a person’s phone number is not considered PHI is false.9. If you see other staff violating privacy policies, you should-
A. Ignore it.
-
B. Give them a helpful, gentle reminder
-
C. Report problems and violations
-
D. Both answer B & C
Correct Answer
D. Both answer B & CExplanation
If you see other staff violating privacy policies, it is important to take action rather than ignoring it. Giving them a helpful, gentle reminder can be a good approach to address the issue informally and remind them of the importance of privacy policies. However, if the violation continues or is more serious, it is necessary to report the problems and violations to the appropriate authorities or supervisors. Therefore, the correct answer is both B and C, as both options involve taking action to address and report privacy policy violations. -
-
10. You work in the billing department of your agency, and while processing claims, you notice the name of someone you know. Since you are curious, you decide to investigate, and you pull their medical record and read it. Is this appropriate?
-
A.Yes
-
B.No
Correct Answer
B. NoExplanation
No, it is not appropriate to investigate and read someone’s medical record without a legitimate reason or proper authorization. Accessing someone’s medical information without their consent is a violation of their privacy rights and breaches confidentiality. In this scenario, the individual’s personal connection does not justify the intrusion into their medical records. It is important to respect and uphold patient confidentiality and only access medical records for legitimate and authorized purposes.11. You receive a call from staff at a local hospital stating that they need information regarding a former client of yours who is scheduled for surgery. They fax you a release of information form that only authorizes the release of medications, but the person on the phone is asking for dates of treatment and diagnoses. How would you respond?-
A. Tell them everything they need to know because they are calling from a hospital
-
B. Release information regarding medications only
-
C. Refuse to release any information
-
D. None of the above
Correct Answer
B. Release information regarding medications onlyExplanation
The correct answer is to release information regarding medications only. The release of information form specifically authorizes the release of medications, not dates of treatment and diagnoses. Therefore, it is important to adhere to the limitations outlined in the form and only provide the requested information.12. Results of tests/procedures can be made available to the client’s family if the client is unable to communicate well.-
A. True
-
B. False
Correct Answer
B. FalseExplanation
The statement is false because the results of tests/procedures cannot be made available to the client’s family solely based on the client’s inability to communicate well. The release of medical information is governed by strict privacy laws and regulations, such as HIPAA in the United States. In order to share medical information with the client’s family, proper consent or legal authorization is required, regardless of the client’s communication abilities.13. Each state has the same laws, rules, and/or regulations governing the confidentiality of health care information.-
A. True
-
B. False
Correct Answer
B. FalseExplanation
The statement is false because each state has its own laws, rules, and regulations regarding the confidentiality of health care information. These laws can vary from state to state, so it is not accurate to say that all states have the same regulations in place. -
-
4. The Federal Regulations on Confidentiality of Alcohol and Drug Abuse Patient Records is one example of
-
A. Confidentiality
-
B. Release of information
-
C. Preemption
-
D. All of the above
Correct Answer
C. PreemptionExplanation
The Federal Regulations on Confidentiality of Alcohol and Drug Abuse Patient Records is an example of preemption. Preemption refers to a situation where a federal law takes precedence over state or local laws on the same subject matter. In this case, the federal regulations on confidentiality of patient records preempt any conflicting state or local laws, ensuring uniformity and consistency in the protection of patient confidentiality across the country.15. It is NOT important to read and understand your agency’s Notice of Privacy Practices.-
A. True
-
B. False
Correct Answer
B. FalseExplanation
The correct answer is False. It is important to read and understand your agency’s Notice of Privacy Practices. This document outlines how your personal information will be used, stored, and shared by the agency. It also informs you of your rights regarding your personal data. By reading and understanding this notice, you can make informed decisions about your privacy and take necessary steps to protect your personal information. -
-
6. Each healthcare provider MUST have a document that describes how information about the client is used by the agency and when the agency will disclose/release it without the client’s authorization.
-
A. True
-
B. False
Correct Answer
A. TrueExplanation
Each healthcare provider is required to have a document that outlines how client information is used and when it can be disclosed without the client’s authorization. This document is important for ensuring transparency and protecting the privacy of clients. It helps to establish clear guidelines and protocols for the handling of sensitive information, ensuring that it is only shared when necessary and in accordance with legal and ethical standards. By having this document in place, healthcare providers can demonstrate their commitment to safeguarding client confidentiality and maintaining trust in the healthcare system.17. If a state or federal law or regulation grants the client greater access to their PHI, then it will preempt HIPAA.-
A. True
-
B. False
Correct Answer
A. TrueExplanation
If a state or federal law or regulation grants the client greater access to their Protected Health Information (PHI), it means that the client has more rights and privileges regarding their health information than what is provided by HIPAA (Health Insurance Portability and Accountability Act). In this case, the state or federal law will take precedence over HIPAA, making the statement true. This implies that if a client’s access rights are expanded by a law or regulation, HIPAA regulations will not restrict or limit their access to their PHI. -
-
18. Substance abuse regulations do not allow disclosure with a subpoena unless a court has issued an order following a show cause hearing.
-
A. True
-
B. False
Correct Answer
A. TrueExplanation
Substance abuse regulations typically prioritize the confidentiality of individuals seeking treatment for substance abuse. As a result, disclosing information related to substance abuse with a subpoena is generally not allowed unless a court has issued an order after a show cause hearing. This ensures that the individual’s privacy rights are protected and that any disclosure is done in a legally appropriate manner. Therefore, the statement is true. -
-
19. A release of information must include which of the following?
-
A. Clients name
-
B. A description of information to be disclosed
-
C. An expiration date
-
D. A description of the purpose of disclosure
-
E. All of the above.
Correct Answer
E. All of the above.Explanation
A release of information must include all of the above because it is necessary to include the client’s name to identify who the information is being released for. A description of the information to be disclosed is important to specify what exactly is being released. An expiration date is necessary to establish a time limit for the release of information. Lastly, a description of the purpose of disclosure is important to provide clarity on why the information is being released. -
-
20. Privacy and security include which of the following best practices?
-
A. Talking about consumers in public areas or where you can be overheard
-
B. Sharing your computer password with a new staff that does not have their own
-
C. Including PHI in an unencrypted email via a public system
-
D. Keeping computer screens out of sight of others
-
E. None of the above
Correct Answer
E. None of the aboveExplanation
The given correct answer is “None of the above.” This is because all of the options listed in the question are examples of poor privacy and security practices. Talking about consumers in public areas or where you can be overheard, sharing your computer password with someone who does not have their own, and including PHI (Protected Health Information) in an unencrypted email via a public system all pose risks to privacy and security. Keeping computer screens out of sight of others is a good practice, but it is not listed as an option in the question. -
Basic HIPAA Quiz: Test!

The health insurance portability and accountability act is a federal law that inhibits access to private medical information. For this quiz, you need to be conscious of who must abide by HIPPA rules and regulations, the best way to secure your password, what health information is, and what was important about the HITECH and Omnibus Rule. If you need to know about HIPPA, this is the quiz for you.
Questions and Answers
-
1. Who must abide by HIPAA rules and regulations?
-
A. Both business associates and covered entities
-
B. Covered Entities only
-
C. Business Associates only
-
D. Either business associates or covered entities
Correct Answer
A. Both business associates and covered entitiesExplanation
Both business associates and covered entities must abide by HIPAA rules and regulations. Covered entities include healthcare providers, health plans, and healthcare clearinghouses, while business associates are individuals or organizations that provide services to covered entities and have access to protected health information. HIPAA rules aim to protect the privacy and security of patients’ health information and require compliance from both covered entities and their business associates to ensure the confidentiality of sensitive data. -
-
2. What is HIPAA?
-
A. A regulation to combat waste, fraud, and abuse in the health care setting
-
B. An act to amend and improve the portability of health insurance coverage
-
C. Game played by employees
-
D. A rule to set standards with respect to the rights of individuals to their health information
Correct Answer
B. An act to amend and improve the portability of health insurance coverageExplanation
HIPAA stands for the Health Insurance Portability and Accountability Act. It is an act that aims to improve the portability of health insurance coverage, allowing individuals to maintain their insurance coverage even when they change jobs or have pre-existing medical conditions. It also establishes standards to protect the privacy and security of individuals’ health information, ensuring that their personal health data is kept confidential and secure. -
-
.3 . Which of the following are best practices for securing your password?
-
A. Never share your password with anyone
-
B. Creating passwords that are only lower case letters.
-
C. Do not post or save your password where others can find it
-
D. If you are asked for your password by a friend, you share it with them.
Correct Answer
A. Never share your password with anyoneExplanation
The best practice for securing your password is to never share it with anyone. Sharing your password with others increases the risk of unauthorized access to your accounts and personal information. It is important to keep your password confidential and not disclose it to anyone, even if they are a friend or acquaintance. By following this practice, you can maintain the privacy and security of your accounts. -
-
4. What is Health information?
-
A. The past, present or future physical/mental health or condition of an individual
-
B. Created or received by an healthcare professional
-
C. The health information of the pet of a patient.
-
D. Payment provision of healthcare to an individual.
Correct Answer
A. The past, present or future physical/mental health or condition of an individualExplanation
Health information refers to the past, present, or future physical/mental health or condition of an individual. This information is typically created or received by a healthcare professional and is used to provide healthcare services to the individual. It does not include the health information of a patient’s pet or the payment provision of healthcare. -
-
5. Potential security incidents are:
-
A. Correct patient name
-
B. Correct physician ID
-
C. Incorrect template use
Correct Answer
C. Incorrect template useExplanation
The potential security incidents mentioned in the question are “Correct patient name” and “Correct physician ID”. These incidents refer to situations where patient names and physician IDs are handled correctly, indicating that there is no security breach in terms of identifying the correct individuals. However, the third potential security incident mentioned is “Incorrect template use”. This suggests that there might be a misuse or mishandling of templates, which could lead to security vulnerabilities or breaches in the system. -
-
6. If a Breach occurs, this must be reported immediately.
-
A. True
-
B. False
Correct Answer
A. TrueExplanation
In the given statement, it is stated that if a breach occurs, it must be reported immediately. This implies that reporting a breach is necessary and should be done without delay. Therefore, the correct answer is True, indicating that it is indeed true that a breach must be reported immediately. -
-
7. IIHI is a subset of Health Information.
-
A. True
-
B. False
Correct Answer
A. TrueExplanation
IIHI stands for Individually Identifiable Health Information, which refers to any health information that can be used to identify an individual. Health Information, on the other hand, is a broader term that includes any information related to an individual’s health. Since IIHI is a subset of Health Information, the statement “IIHI is a subset of Health Information” is true. -
-
8. Which of the following comply with HIPAA regulations?
-
A. Do not tell friends or family about patients
-
B. Do not discuss PHI in public areas
-
C. A breach need not be reported.
-
D. Passwords can be shared with friends.
Correct Answer
B. Do not discuss PHI in public areasExplanation
The statement “Do not discuss PHI in public areas” complies with HIPAA regulations because it ensures that protected health information (PHI) is not disclosed or shared in public places where unauthorized individuals may overhear or access it. HIPAA regulations require healthcare providers and organizations to safeguard PHI and maintain its confidentiality, and discussing it in public areas would violate these regulations. -
-
9. HIPAA stands for?
-
A. Healthcare Insurance Portability and Accountability Act.
-
B. Health Portability Act.
-
C. Health Insurance Portability and Accountability Act.
Correct Answer
C. Health Insurance Portability and Accountability Act.Explanation
HIPAA stands for Health Insurance Portability and Accountability Act. This act was enacted in 1996 to ensure the privacy and security of individuals’ health information. It provides guidelines and regulations for healthcare providers, health plans, and other entities that handle protected health information. The act also aims to promote the portability of health insurance coverage and prevent fraud and abuse in the healthcare industry. -
-
10. What was important about the HITECH and Omnibus rule?
-
A. Strengthened HIPAA requirements and expanded the rights of individuals under HIPAA.
-
B. Easy to access patient protected information
-
C. Transportation between healthcare facilities
-
D. Strengthened the power of hospitals.
Correct Answer
A. Strengthened HIPAA requirements and expanded the rights of individuals under HIPAA.Explanation
The HITECH (Health Information Technology for Economic and Clinical Health) and Omnibus rule were important because they strengthened the requirements of the Health Insurance Portability and Accountability Act (HIPAA) and expanded the rights of individuals under HIPAA. These rules aimed to enhance the privacy and security of patient health information, promote the adoption of electronic health records, and increase transparency in healthcare practices. By strengthening HIPAA requirements, the rules aimed to ensure that healthcare organizations and providers are taking appropriate measures to protect patient data and giving individuals more control over their health information. -
.
Send Stories | Social Media | Disclaimer
Send Stories and Articles for publication to [email protected]
We Are Active On Social Media
WhatsApp Channel: JOIN HERE
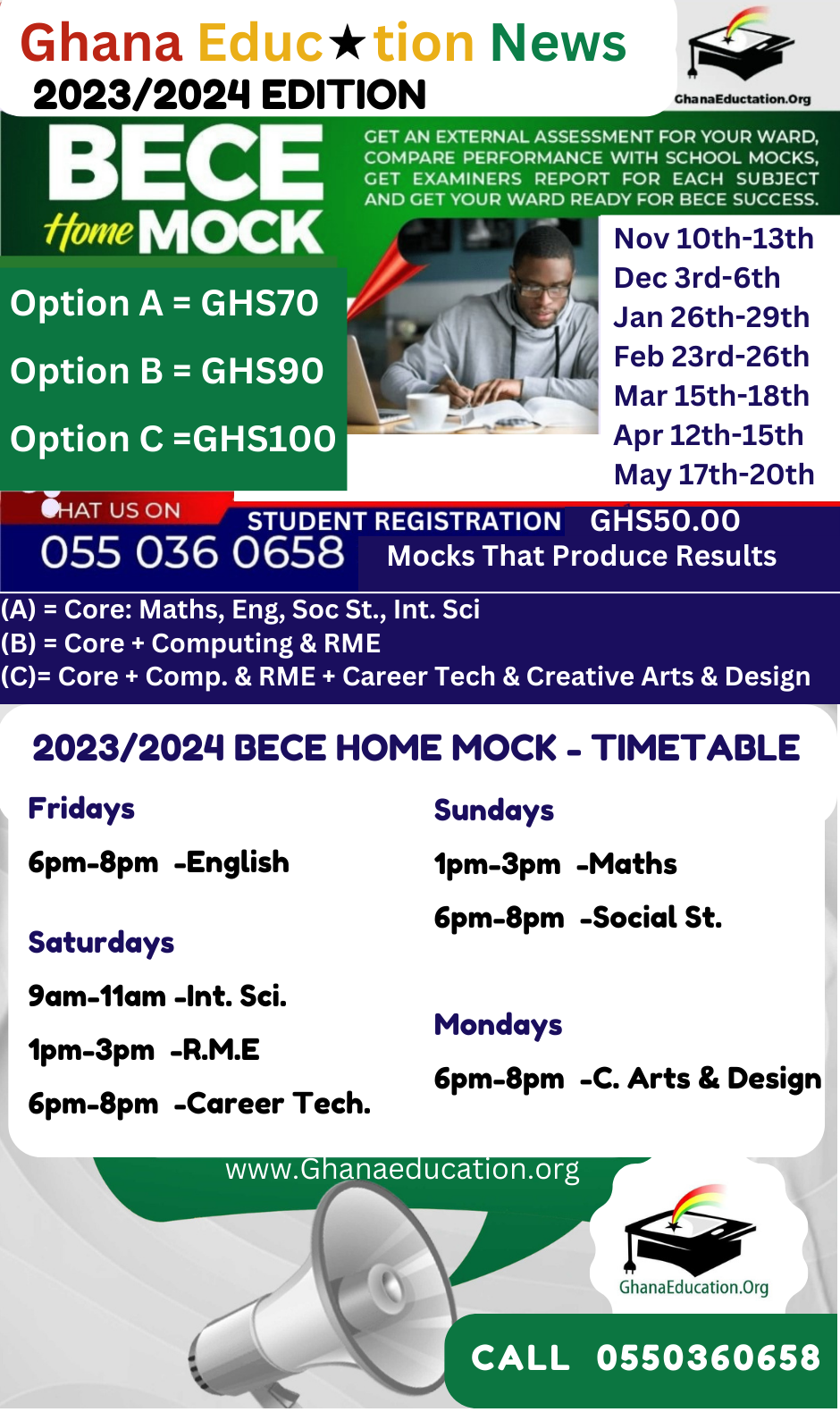
2024 BECE and WASSCE Channel - JOIN HERE
Facebook: JOIN HERE
Telegram: JOIN HERE
Twitter: FOLLOW US HERE
Instagram: FOLLOW US HERE
Disclaimer:
The information contained in this post on Ghana Education News is for general information purposes only. While we endeavour to keep the information up to date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability or availability with respect to the website or the information, products, services, or related graphics contained on the post for any purpose.


 How to buy UG Admission Voucher with Momo/Shortcode
How to buy UG Admission Voucher with Momo/Shortcode  Top 5 Universities in the Netherlands for Masters Studies
Top 5 Universities in the Netherlands for Masters Studies  John Mahama Lists Plans for Education Sector When he is Voted for
John Mahama Lists Plans for Education Sector When he is Voted for  The Poll Tax Ordinance of 1852
The Poll Tax Ordinance of 1852  Asogli State rejects renaming Ho Technical University after Ephriam Amu
Asogli State rejects renaming Ho Technical University after Ephriam Amu